Follow Us!
Patient stories, informative videos and much more on our social media accounts
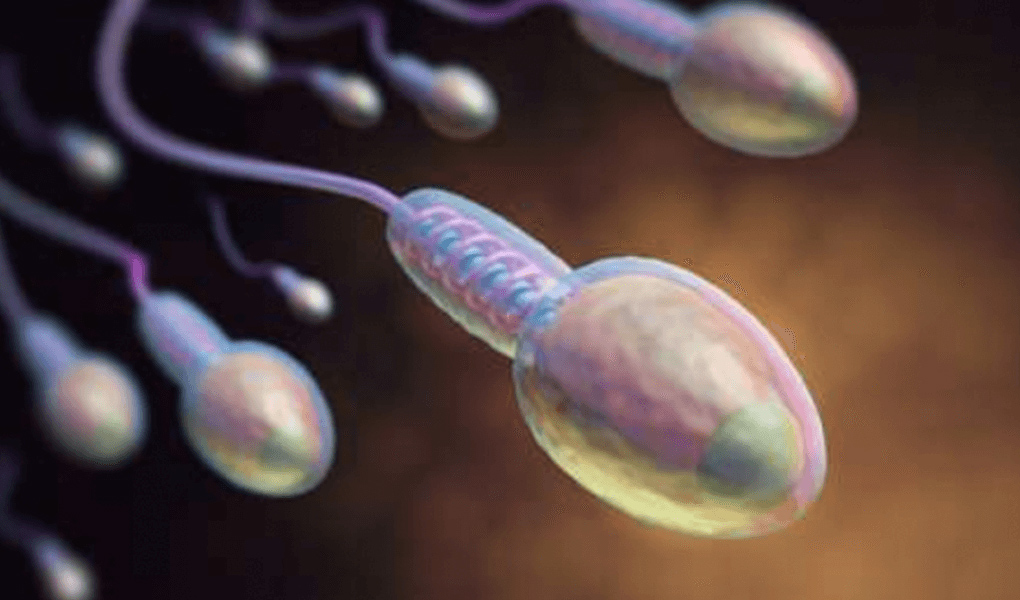
Male infertility is a growing concern worldwide, and semen analysis is one of the first diagnostic tests requested when couples experience difficulty conceiving. Among the parameters evaluated in semen analysis—sperm count, motility, and morphology—sperm morphology disorders are often the most misunderstood and underestimated factor.
While many men focus primarily on sperm count, scientific evidence shows that sperm morphology plays a critical role in fertilization, embryo development, and pregnancy outcomes, particularly in assisted reproductive treatments such as IVF and ICSI.
Sperm morphology refers to the shape and structural integrity of sperm cells. A normal sperm cell must have a properly formed head, neck (midpiece), and tail to successfully fertilize an egg.
Sperm morphology is evaluated using internationally accepted criteria, most commonly:
During evaluation, sperm cells undergo special staining and preparation, then are examined under high magnification to assess abnormalities in:
Only sperm cells that meet all structural criteria are classified as normal morphology.
In many routine semen analyses, emphasis is placed on sperm count and motility. However, recent clinical studies show that morphology may be more predictive of fertilization success than count or motility alone.
This is because:
According to Kruger criteria, as little as 4% normal morphology is considered acceptable, meaning that up to 96% abnormal sperm can still be classified as “normal.” This surprises many patients but reflects how strict morphology assessment truly is.
A healthy sperm cell consists of three distinct parts:
Normal measurements:
Abnormalities in the head can affect DNA integrity and the ability to penetrate the egg.
Defects in this area reduce motility and fertilization capacity.
Normal tail length: approximately 40–50 µm
Tail abnormalities may cause poor motility even if sperm count is normal.
Some of the most frequently observed sperm deformities include:
Certain deformities, such as globozoospermia, are associated with severe fertilization failure, even with IVF, and require advanced laboratory techniques.
Poor sperm morphology can lead to:
In natural conception, severely abnormal morphology may significantly prolong the time to pregnancy. In assisted reproduction, morphology guides the choice of treatment method.
Morphological assessment plays a critical role in assisted reproductive techniques:
In cases of severe morphology disorders, ICSI is often the preferred method, allowing embryologists to select the best available sperm.
For specific deformities (e.g., globozoospermia), additional laboratory precautions and activation techniques may be required to achieve fertilization.
One of the most common questions patients ask is:
“Can sperm morphology be corrected?”
The answer depends on the cause.
Some morphology defects may improve if caused by:
Eliminating these factors may improve overall sperm quality over time.
To date, no supplement has been proven to reliably correct sperm shape disorders.
However, antioxidants and micronutrients may:
Therefore, supportive treatments may benefit overall sperm quality, even if morphology itself remains unchanged.
Men should consult an andrology or fertility specialist if:
Early evaluation allows personalized treatment planning and improves success rates.
According to Kruger criteria, ≥4% normal forms is considered acceptable.
Yes, but the probability may be reduced depending on severity.
In many cases, yes—especially for fertilization success.
Severe abnormalities may be associated with higher DNA damage and pregnancy loss.
Not always, but it is commonly recommended in severe cases.
Sperm morphology disorders represent one of the most complex and critical aspects of male infertility. While often overlooked, morphology provides invaluable insight into sperm function, fertilization potential, and treatment planning.
Although not all morphology defects can be corrected, modern reproductive technologies and individualized laboratory approaches allow many men with severe sperm morphology disorders to become fathers.
If you have concerns about sperm morphology or fertility, consulting an experienced fertility center is the most effective step toward a successful outcome.
Let us call you as soon as possible regarding the issues you want to consult.